10 Dysphagia Resources that Promote Patient Choice
Every medical choice comes with pros and cons, risks and benefits. It’s our job to outline what these are and then to step back and support patient choice.
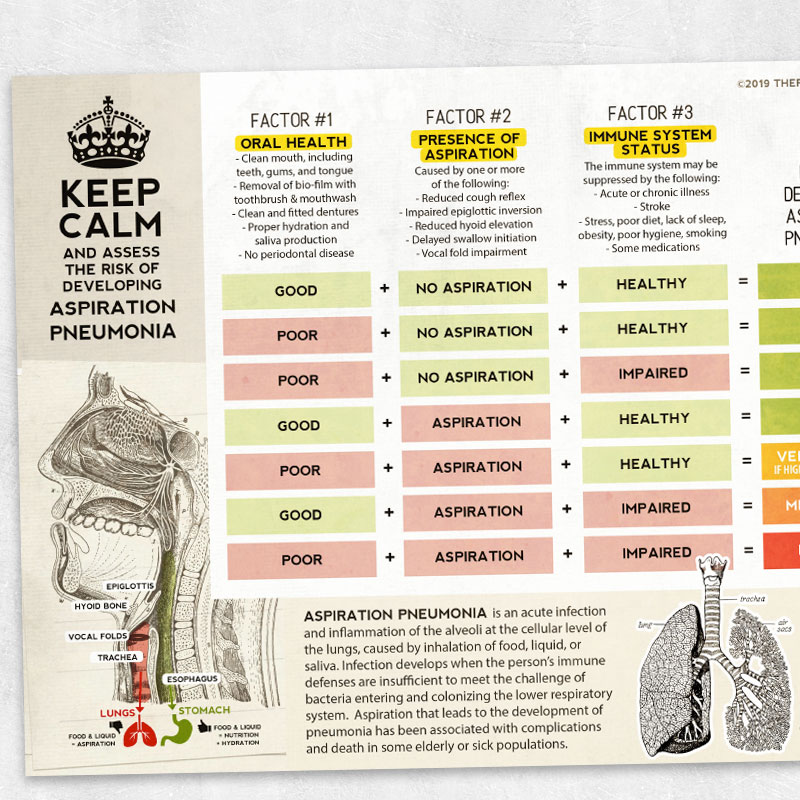
Not everyone who aspirates will develop a lung infection. This is the basis of the fantastic explorations of John Ashford, PhD, SLP. You can find his important work here. In a nutshell, the development of aspiration pneumonia depends on a variety of factors that are unique to each individual person. While we can never perfectly predict the risks, we can make some informed hypotheses and discuss these factors with our patients.
Resource #1: Keep Calm and Assess the Risk of Developing Aspiration Pneumonia
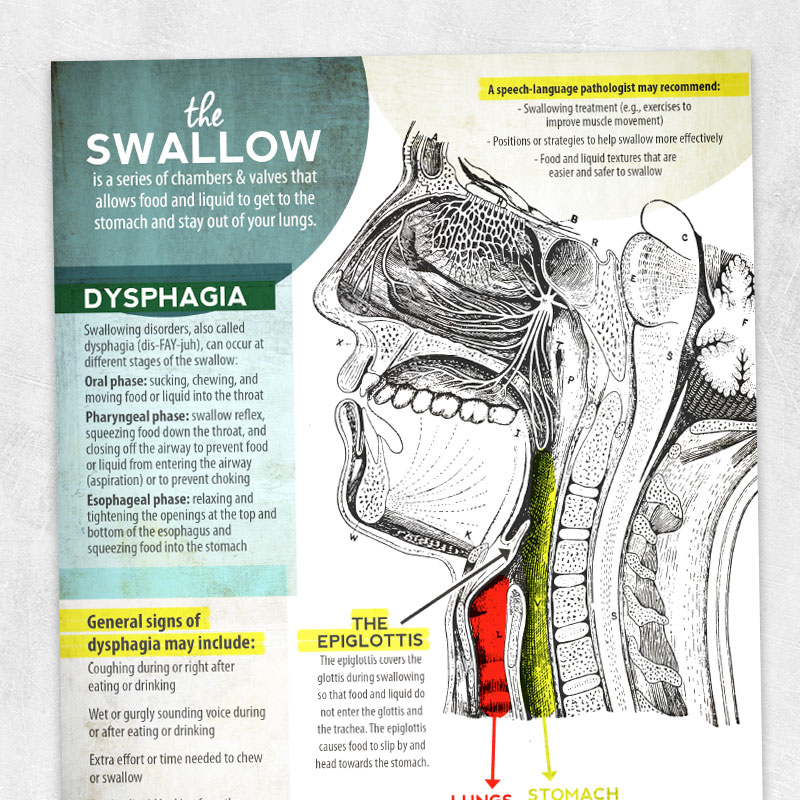
We have access to an entire graduate level course on dysphagia anatomy and physiology. Our patients have only a few minutes to figure it out.
Even though we all swallow thousands of times per day, it’s not a process that intuitively makes a lot of sense. For some of us, it can help to visualize what is going on inside our bodies in order to better understand what is working and what isn’t. This visual pairs particularly well with lateral-view VFSS.
Resource #2: The Swallow
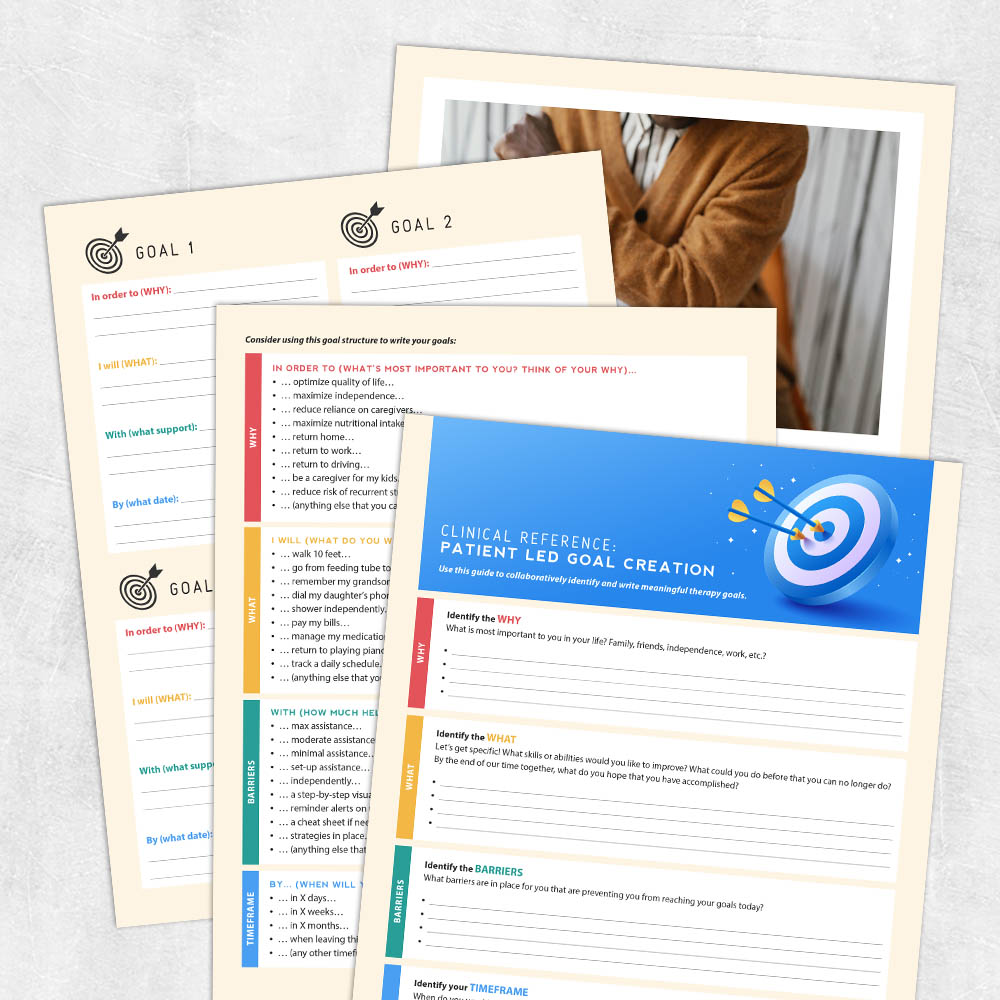
When we measure progress, the person should be defining what progress means and how we measure it.
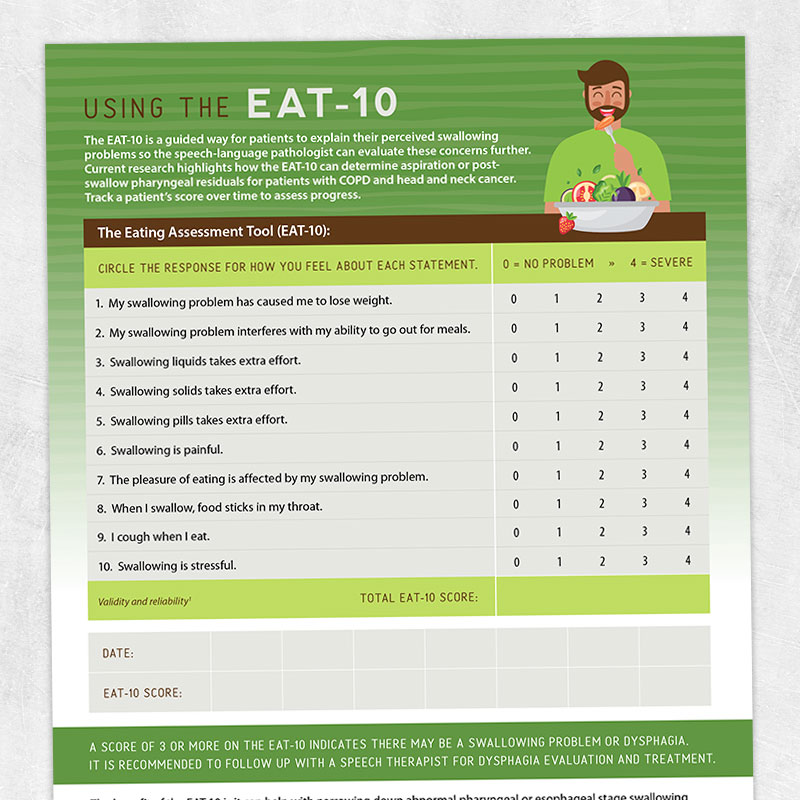
The tools we use to measure the severity of the dysphagia should include the perceptions of the person (such as the EAT-10). When we write goals, we can collaborate with the patient to understand their unique values, priorities, and goals. While this isn’t always possible, depending on cognitive status, we can implement collaborative goal writing whenever possible.
Resource #3: Using the EAT-10
Resource #4: Patient-Led Goal Creation
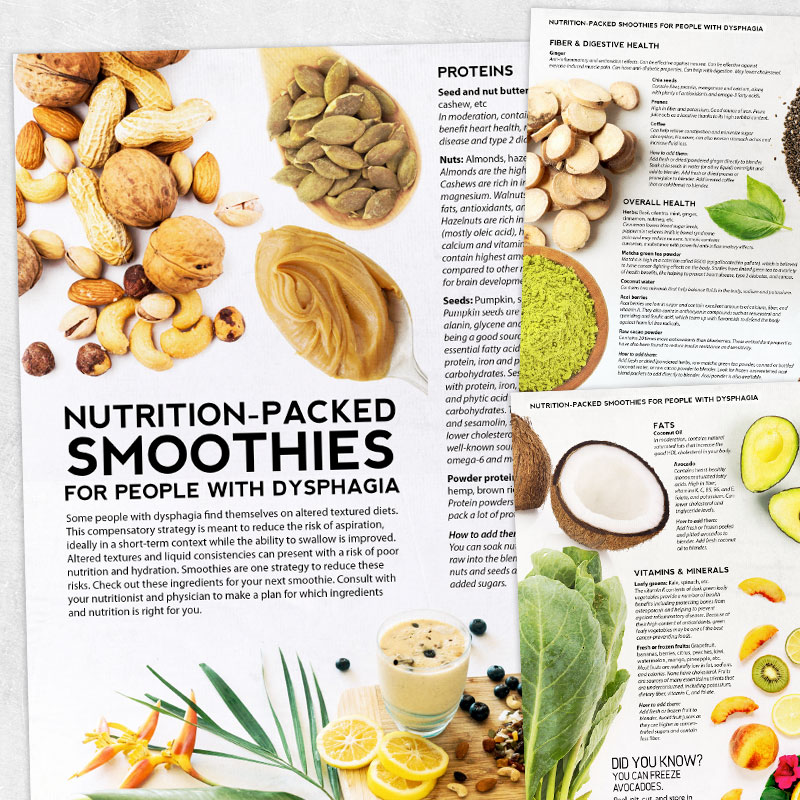
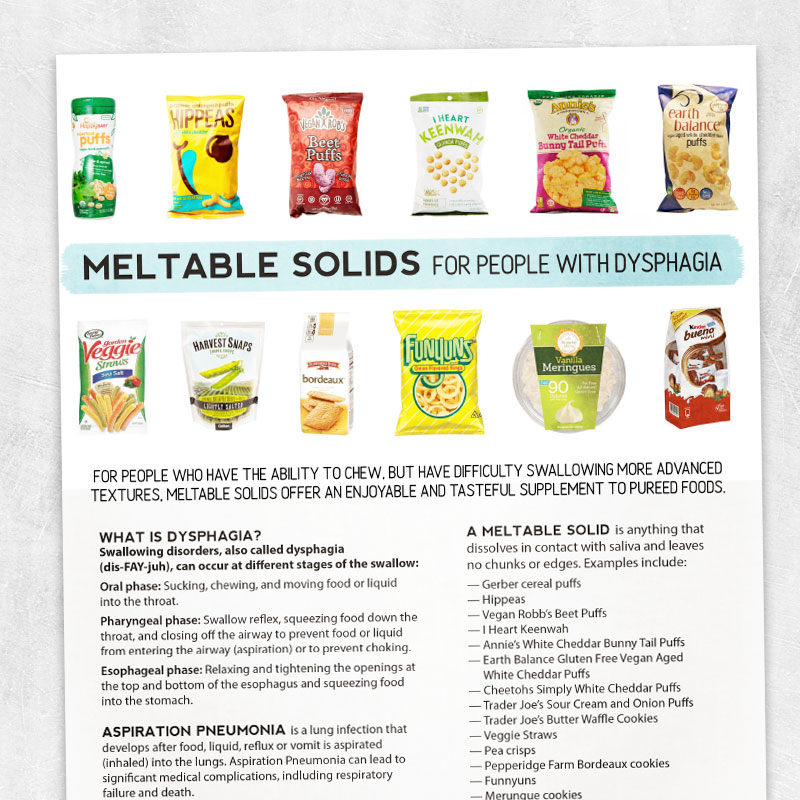
If someone chooses to change their diet texture, we can bring a lot of creative ideas to the table to ensure that food is still enjoyable and nutritious.
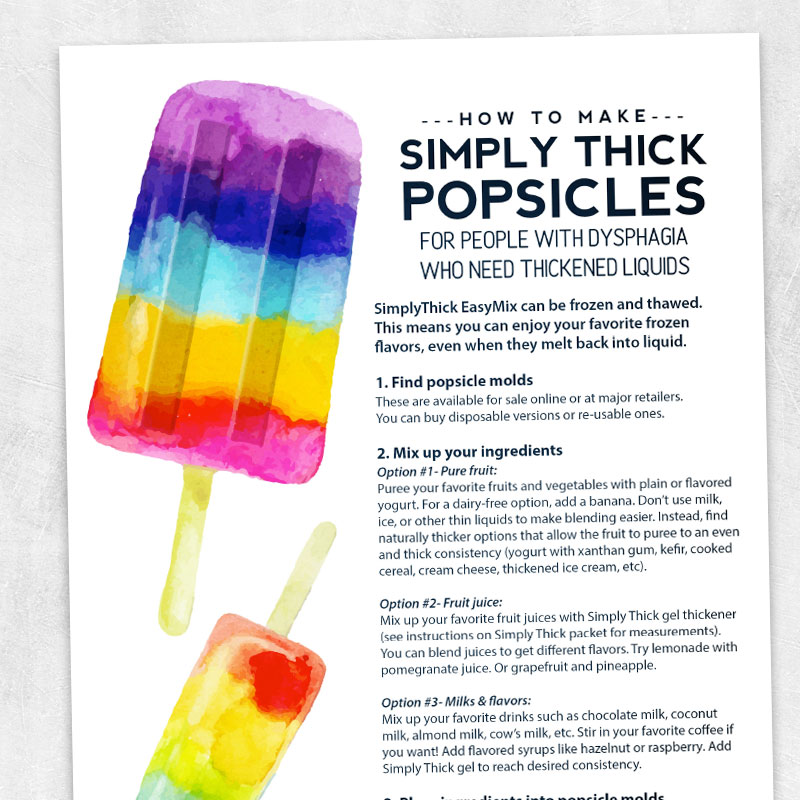
If we work in a facility, we can build relationships with the culinary staff and dietitian team, advocating for people to get delicious, nutritious foods that meet their altered diet texture needs. If we work with people in their home environments, therapy can focus on preparing these foods in ways that meet the altered texture requirements. We can bring some flavor power to mashed potatoes, blend nutrition-packed smoothies, explore meltable solids, or make some cold, refreshing, thirst-quenching thickened-liquid popsicles on a hot day. No one should have to suffer with food that looks like gelatinous blobs. Our role here leans heavily into advocacy, creativity, and collaboration!
Resource #5: Nutrition-Packed Smoothies for People with Dysphagia
Resource #6: Puree Flavor Power: 27 Ways to Get Creative with Mashed Potatoes
Resource #7: Meltable Solids for People with Dysphagia
Resource #8: How to Make Simply Thick Popsicles

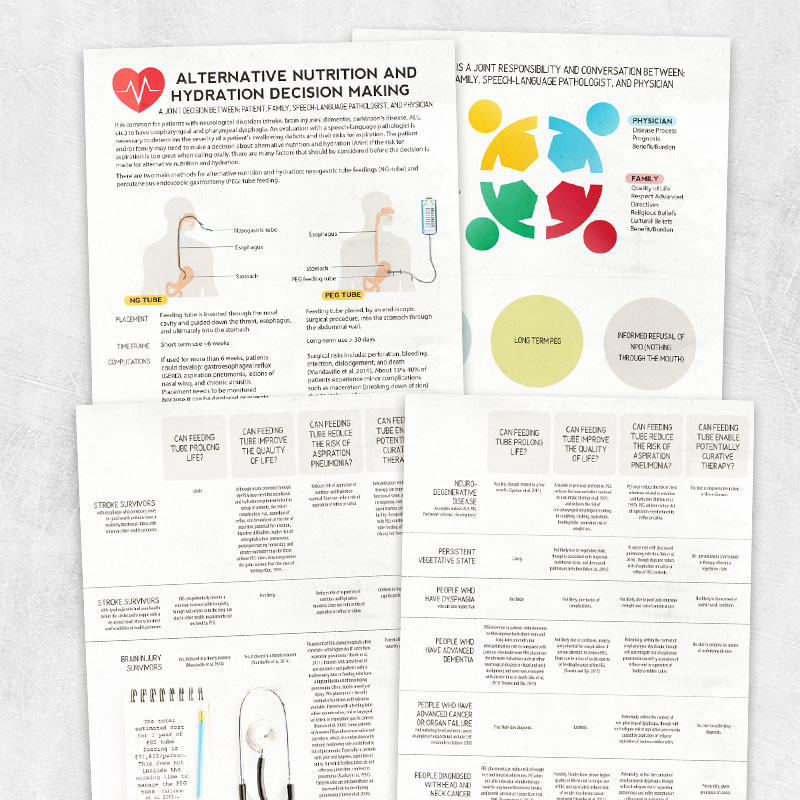
Deciding to go the route of alternative nutrition and hydration is a deeply personal decision that requires collaboration and discussion that weighs all of the pros and cons.
In acute situations, tube feedings may be the only viable option for survival. In other situations, the option of alternative nutrition and hydration can come up for a variety of reasons, including refusal to eat, unmanageable weight loss, severe dysphagia, cognitive impairments, and other medical reasons. Our role is key here, as these alternative methods don’t always deliver the quality of life that many of us assume they will. Sharing resources that break down the pros and cons can help patients and families decide what is best for them. Regardless of the decision, we support what the person and their family decides.
Resource #9: Alternative Nutrition and Hydration Decision Making
Food provides a lot of joy, connection, and comfort to all of us, whether we’re enjoying it or preparing and sharing it. When it’s no longer a comfort, SLPs can hold space for embracing this hard truth.
Sometimes, the choice isn’t about what to eat or how to eat it; it’s about whether to continue to expect someone to eat or not. SLPs play an enormously important role at this juncture. It can feel cruel to stop feeding someone that we love. Sometimes we need more information to understand how this is part of the natural process of aging and dying. Sometimes person-centered care requires us to be an advocate for patients who are trying to communicate their preferences without speaking.
Resource #10: When Food is No Longer a Comfort
Evidence-based care is not just about what has been published in the research. It requires factoring in your own clinical experience as well as the unique goals and values of each individual patient.
Let me paint an example: A man experiences a cervical spinal cord injury and is wearing a neck collar, coughing on everything he tries to drink. A video study reveals trace aspiration on only one trial of a series of trials across consistencies. No postural maneuvers helped (always tricky when you can’t really move your neck!), but mildly thickened liquids did.
What would science tell us to do? What does the patient want? And which one of these guides the overall conversation? None of this is cut and dry.
One question I get a lot is: Ok, Megan, this is all great, but how do you even document this? Isn’t my job to keep the patient safe? If they aren’t going to choose to be safe, doesn’t that put my license on the line?
Here’s a thought to ponder: An oncologist would never force a patient to get chemotherapy or radiation in order to “save their medical license.” That’s a wild idea!
Likewise, we shouldn’t be forcing people to follow strict diet recommendations. Our job is to advocate, educate, and support, not to dictate, enforce, and punish.
Here are some quick tips for your documentation:
- Describe the dysphagia in medical terms: Pt presents with pharyngeal dysphagia characterized by aspiration of thin liquids as seen on VFSS with sole effective strategy of mildly thick liquids reducing risk of aspiration. No aspiration risk noted with any other textures of food/liquid. No oral dysphagia noted. Current status related to recent cervical SCI. Interdisciplinary discussions note that dysphagia could possibly be related to edema s/p surgery with team recommendation to monitor in the coming weeks for resolution.
- Describe your education: Discussed results of VFSS with patient, including replaying x-ray video, discussing anatomy and physiology of swallow with visuals, exploring the risk factors of developing aspiration pneumonia in the setting of acute dysphagia, and options for more enjoyable drinks if the patient elects to alter his liquid consistency.
- Describe the patient choice: At this time, the patient is electing to consume thin liquids with consistent, thorough oral care and basic swallow precautions. Pt verbalized understanding of the risks involved, and he and our interdisciplinary team are collaborating to reduce those risks and support his plan of care.
Here’s a quick list of check-in questions you can ask yourself if you want to work on moving towards person-centered care:
- What false assumptions am I making about this patient and/or this situation?
- Am I valuing what the research says is “safe” or “right” over what the patient wants?
- Am I afraid of being wrong? (SLP perfectionist culture, especially online, has zero space for ambiguity, and many SLPs feel that they have to be 100% right 100% of the time, including making “correct” diet recommendations. Just remember that when you’re prioritizing education and patient choice, there is no “wrong” answer).
- If the person’s decision is bringing up challenging feelings for me (frustration, anger, annoyance, etc), what are those feelings about? This might indicate some work to be done around being easier on yourself and your patients. There is no “right” answer in therapy. It’s more about collaboration, respect, dignity, choice, and compassion.
Dysphagia is a relatively new addition to the field of speech-language pathology and we are all learning and growing as we go. We would love to hear your thoughts! Drop a comment at the end of this article or reach out to us any time.